When we work with patients with pain, one of our goals is to figure out what is the main cause or “driver” of your symptoms, in order to have an optimal treatment outcome. A “driver” can be due to an illness, tissue injury or nervous system dysfunction, and in many cases there is more than one (especially once the pain becomes chronic). For example, the initial driver for a woman’s pelvic pain could be an endometriosis diagnosis. Pain can arise from the abnormal endometrial growth in the pelvic region. Unfortunately, the body’s response to this pain, such as holding chronic tension in the pelvic muscles, can create more pain- so now there is more than one driver. A similar example would be the prostatitis diagnosis for men.
Pain can also be driven by repetitive activity or traumatic injury- such as a cyclist with pelvic pain due to pressure from bike seat, or a soccer player with testicle pain due to a groin injury. Some occupations can also contribute to the onset of pain – prolonged sitting at a computer or in truck seat, heavy lifting, even a highly stressful environment that contributes to chronic muscle tension. There are many causes of this type of tissue driven pain.
Our own nervous system can also be part of the problem. We describe some patients as having an “upregulated” nervous system. In this case, the nerves that carry the signals from your body up to the brain have become extra sensitive, and now even light touch, simple movement, or the even the pressure of your clothing becomes painful. This can happen to some people following injury or surgery, as well as from chronic yeast infections or repetitive UTI’s.
Common words used to describe pelvic pain include:
Interstitial Cystitis (IC)
Painful Bladder syndrome
Vulvodynia
Vulvar Vestibulitis
Vaginismus
Dypareunia (painful intercourse)
Pudendal neuralgia
Sacroiliac dysfunction
Dysuria- pain with urination
Dyschezia- pain with bowel movments
Pubalgia
Rectal pain/ anismus
Orchalgia (testicle pain)
Prostatitis
Ejaculatory pain, dysfunction
Pudendal neuralgia
Sacroiliac dysfunction
Dysuria- pain with urination
Dyschezia- pain with bowel movments
Pubalgia
Rectal pain/anismus
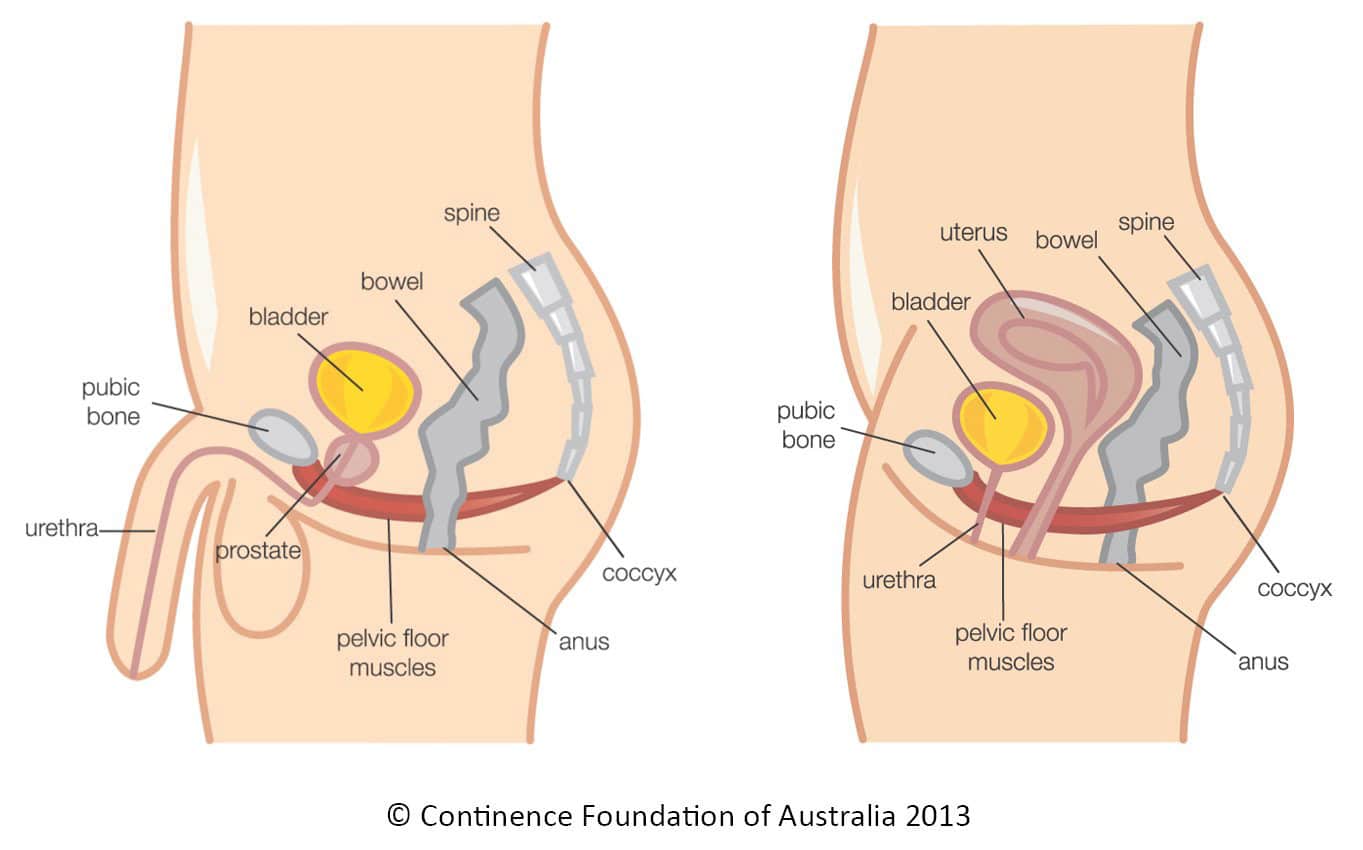
The muscular and nerve imbalance due to pelvic floor dysfunctions can also effect bladder and bowel function. Symptoms may include an irritating sense of urinary urgency or abnormally frequent trips to toilet, difficulty starting the flow of urine, constipation, and excessive straining. It could contribute to a sense of incomplete emptying for bowel or bladder, or even painful evacuation.
Once your doctor has determined that there is no active infection or disease causing your symptoms, our pelvic physical therapy can help to diminish and possibly eliminate your pain and associated bowel and bladder dysfunctions.
Physical therapy will involve an assessment of the pelvic girdle and surrounding muscles. We will help you learn how to manage and decrease your pain, relax chronic tension, empty your bladder or bowel without straining, strengthen and improve muscle control, give guidelines and suggest lifestyle modifications that will help you recover function and get your life back.
Some things you can do on your own:
- Recognize that a muscle spasm is something that can be corrected. Stress is known to make muscle spasms worse, so learning to relax can be very helpful to reduce your pain and/ or bladder irritation. Diaphragmatic breathing can be helpful to calm down your stress reactions. Take several deep breaths (expand your belly and chest with a breath in) several times a day.
- Take a hot bath (or use a hot pack on your pelvic floor and bladder) every day. Just as you would put heat on a chronically tense back muscle, using heat on chronically tense pelvic muscles can help.
- If sitting increases your pain, frequently stand and relieve the pressure on this group of muscles as much as you can. Consider purchasing a perineal relief cushion.
- Take appropriate over-the-counter or doctor-prescribed medications.
